Pregnancy monitoring
During the pregnancy, Jane Tisler will monitor and offer you guidance in close cooperation with Dr. Marek Šois. Your next appointment will be scheduled at the end of each visit. You can come to the appointments and ultrasound screenings with a family member or someone close to you.
-
Weeks 6-8 of pregnancy
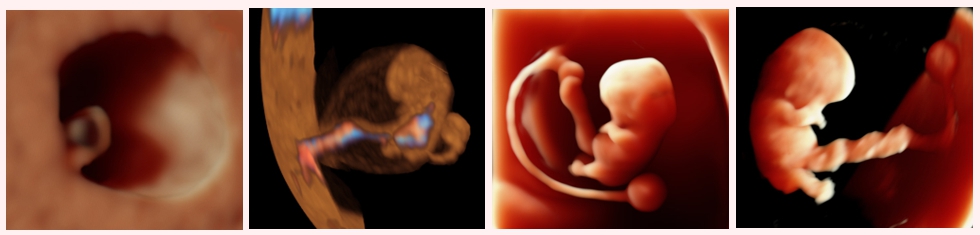
The gynaecologist will confirm how far along you are and your due date with the help of vaginal ultrasound. The viability of the fetus and whether it is a twin pregnancy will also be assessed. The gynaecologist will familiarize you with the Fetal Ultrasound Center’s monitoring program and will provide a complete overview of the screening tests in the first half of the pregnancy and will advise on the need for folic acid intake.
-
Weeks 9-10 of pregnancy

Gynecologists will perform a vaginal ultrasound examination to look for any developmental defects that are incompatible with life and to assess the fetal growth dynamics. During the ultrasound, he will also assess whether there are any contraindications for the performance of non-invasive prenatal testing (NIPT) to look for chromosomal abnormalities. The gynaecologist will also take samples for analysis from the cervix.
After the consultation with the gynaecologist, the midwife or nurse will take a blood sample from you to screen for fetal chromosomal diseases and for early detection of infections (cytomegalovirus infection, toxoplasmosis). If you do not have insurance, you may wish to obtain a certificate to apply for insurance from the Estonian Health Insurance Fund.
-
Weeks 11-12 of pregnancy
Either midwife or nurse will do a set of tests necessary for registering as an expectant mother, which is best done on an empty stomach in the morning between 08:00 and 11:30. It is very important that you do not forget to take a urine sample in the morning.
During that same appointment, your body weight and arterial blood pressure will be measured and a thorough pregnancy history will be taken for the OSCAR test. If you have not been previously diagnosed with the high blood pressure but the blood pressure values measured repeatedly during the appointment exceed the norm, a 24-hour home blood pressure monitoring will be carried out with your consent in order to obtain an objective blood pressure value.
If necessary, you will be advised about any discomforts you may experience during the first half of pregnancy (fatigue, nausea, constipation) and, if you are Rh-negative, the father of your child will be asked to provide a venous blood sample for Rh factor testing.
-
Weeks 12-13 of pregnancy
Gynaecologist and nurse will perform a comprehensive OSCAR test to assess your baby's risk of chromosomal diseases and your risk of preeclampsia, growth restriction and preterm birth, and to check your baby's early development in order to look for possible abnormalities that can be assessed during the given stage of development. After the OSCAR test, your gynaecologist will explain in detail the significance of your test results for the course of your pregnancy and draw up an individual pregnancy management plan for you (pregnancy monitoring plan, possible pregnancy risks, chronic diseases and continuation of daily medication, referral to a specialist).
After the OSCAR test, Midwife will register you as an expectant mother at the Fetal Ultrasound Center. During the appointment, you will be advised of the results of the tests performed, a maternity card will be filled in where your estimated delivery date and maternity leave will be recorded.
The midwife will assess your risk of developing deep vein thrombosis and/or gestational diabetes. For women at risk of gestational diabetes, a time to perform a glucose tolerance test will be agreed upon, and for women at risk of deep vein thrombosis, the midwife will teach you the subcutaneous injection technique and your doctor will issue you a digital prescription for low-molecular-weight heparin.
The midwife will discuss with you the need to get the flu vaccine. The flu season in Estonia is from October to March. Pregnant women are more likely to have a severe case of the flu and develop pneumonia more often than non-pregnant women. With your consent, the midwife will vaccinate you against the flu and fill out and issue you an immunization passport.
During the appointment, the midwife will express interest in the nature of your work (switch to lighter work if necessary), your lifestyle and any harmful habits. The midwife will explain the physiological changes you will experience during pregnancy and offer advice on drinking water, taking supplements and physical activity.
-
Weeks 14-16 of pregnancy
If during the OSCAR test the gynaecologist discovers a risk of spina bifida or congenital heart disease in your child, the gynaecologist will perform a repeat ultrasound examination to rule out suspected pathologies. In monochorionic twins, an ultrasound examination is performed to screen for the presence of early twin-to-twin transfusion syndrome.
If you have previously given birth to a premature baby, or if you have been diagnosed with cervical insufficiency during previous pregnancies, you will undergo a vaginal examination to assess the length of your cervix and the risk of preterm birth. If you are at increased risk of preterm birth, we will discuss with you the need for prophylactic progesterone treatment or cervical cerclage.
If the expectant mother is Rh-negative and the father of the child is Rh-positive or his previous child had an Rh incompatibility and the mother’s blood has Rh antibodies, they will be offered a blood test to assess the child’s Rh factor. A mother whose child is Rh-positive will receive an individual pregnancy monitoring plan for early detection of Rh incompatibility. If you have anti-D, anti-c and Kell system antibodies in your blood, it is important to check for an increase in antibodies once a month.
-
Weeks 20-21 of pregnancy
During the appointment, the midwife will perform a urine test and take a blood sample to assess your levels of haemoglobin. Your body weight and arterial blood pressure will be measured at the appointment.
If the OSCAR test showed that you are at increased risk of preeclampsia, you may want your midwife to perform a blood test to determine the placental growth factor as well, which can be used to reassess the risk of preeclampsia.
During the visit, the midwife will express interest in the nature of your child's movements. If you do not feel the child's movements yet and you are worried about it, it is possible to borrow/purchase a fetal doppler from us. The midwife will teach you how to use the fetal doppler and how to find your baby's heartbeat. The midwife will also familiarize you with the family schools in different maternity hospitals and discuss with you the need for physical activity during pregnancy.
Depending on the level of haemoglobin in your blood, the midwife will assess the need for prophylactic iron replacement therapy.
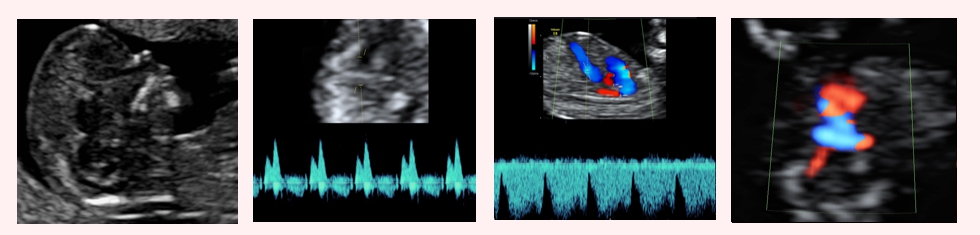
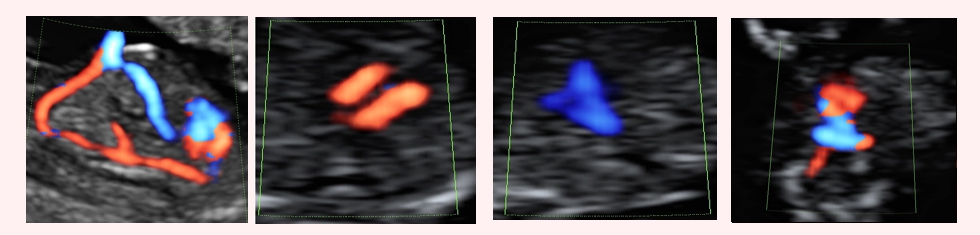
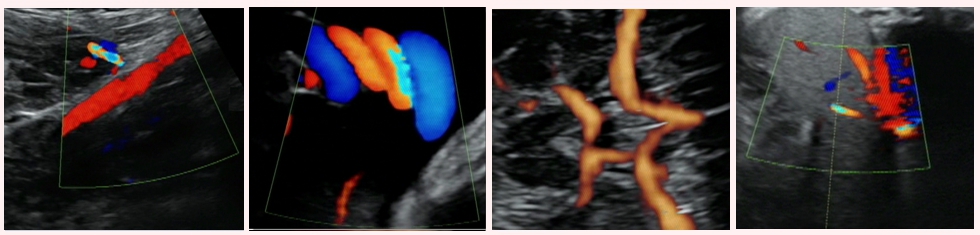
In the second trimester, gynaecologists and nurses will perform an ultrasound screening for fetal developmental defects, during which the development of your child's organ systems will be thoroughly assessed. Particular attention will be paid to the assessment of the child's brain and heart structures. In pregnant women at increased risk of fetal congenital heart disease, echocardiography of the child’s heart will be performed in addition to the anatomical screening. If there is suspicion of a developmental brain defect in the child during an ultrasound examination, a vaginal neurosonography of the child's brain will also be performed in addition to the anatomical screening.
If the OSCAR test showed that you are at an increased risk of preeclampsia, a reassessment of the risk of preeclampsia will be performed to assess the effectiveness of low-dose aspirin prophylaxis and to develop a pregnancy management plan.
If indicated, your gynaecologist will offer you a vaginal ultrasound in order to measure your cervical length and assess the risk of preterm birth. If you have a short cervix and are at increased risk of preterm birth, your gynaecologist will discuss with you the need for prophylactic progesterone treatment.
-
Week 24 of pregnancy
If you are at increased risk for gestational diabetes, or if you have gained excess weight during the pregnancy or if there is sugar in your urine, then midwife will perform a glucose tolerance test to rule out gestational diabetes. To do this, you will have to come to the Fetal Ultrasound Center in the morning on an empty stomach. The midwife will first take a blood sample from you for analysis and ask you to drink a glucose solution, after which blood will be drawn again after 1 hour and 2 hours. If, as a result of the glucose tolerance test, there is a suspicion that you may have gestational diabetes, then midwife will refer you to an appointment with a diabetes nurse.
-
Week 28 of pregnancy

During the appointment, the midwife will perform a urine test and take a blood sample for the analyses in the second half of the pregnancy. If you are Rh-negative and the father of the child is Rh-positive and we do not know if your child is Rh negative or Rh positive, it is necessary to take a venous blood sample and repeat the rhesus antibody assessment. If Rh antigens are not present in your blood, the midwife will discuss with you the need for immune prophylaxis to prevent Rh incompatibility during future pregnancies.
Expectant women may develop very severe cases of pelvic inflammatory disease. Therefore, if you are at risk of urinary tract infection (chronic pelvic inflammatory disease, recurrent leukocytes in the urine), it is important to bring your morning urine with you so that the midwife can send it to the laboratory to test for pathogens.
During the appointment, your body weight and arterial blood pressure will be measured. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema. The midwife will reach an agreement with you on when you will take maternity leave. The midwife will teach you how to recognize the symptoms of preeclampsia. She will discuss with you how to prepare for childbirth. If necessary, you will be advised about any discomforts you may experience during the second half of the pregnancy (heartburn, leg cramps, back pain, constipation).
The midwife will discuss with you the need for pertussis vaccination. Pertussis is an acute respiratory tract infection, characterized by coughing attacks lasting weeks and even months. Pertussis is particularly dangerous for infants, and most deaths are associated with falling ill at under three months of age. Pertussis is one of the causes of sudden infant death syndrome. Studies have shown that the greatest placental transfer of pertussis antibodies to the fetus occurs in the last four weeks of pregnancy. Therefore, it is recommended that pregnant women be vaccinated against diphtheria, tetanus and pertussis during the third trimester of pregnancy. With your consent, the midwife will vaccinate you against pertussis and fill in and issue you an immunization passport.
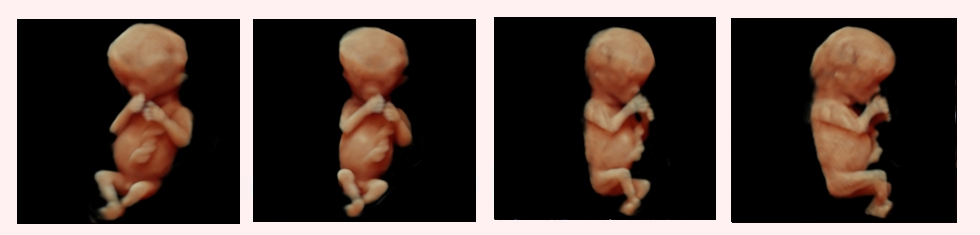
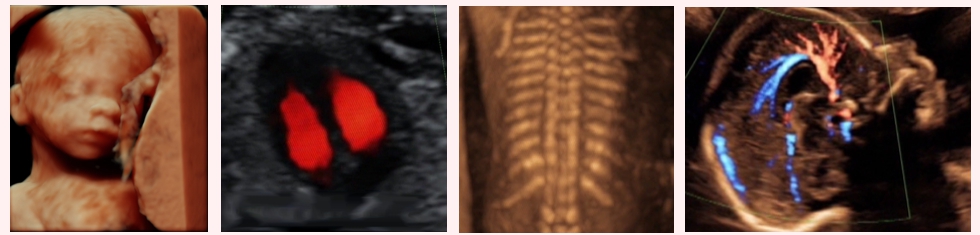
If you long to see your baby, then the 28th week of pregnancy is the best time to come in for a 3D/4D ultrasound for emotional reasons. This far along in the pregnancy, the baby can already open its eyes and its face is already similar to that of a newborn. This far along in the pregnancy, there is the highest chance that there will be enough amniotic fluid between the baby's face and the uterine wall. This allows us to obtain a 3D image of the child's face during the ultrasound. Before coming to the ultrasound, it is recommended to drink more fluids and eat/drink energy-rich food/fluids for the three days before the ultrasound, which increases the likelihood that your child will be awake during the ultrasound and that you will be able to see your child's face as a moving 4D image.
-
Week 32 of pregnancy
During the appointment, the midwife will perform a urine test and take a blood sample to assess the level of haemoglobin in your blood. If your haemoglobin levels are low, your midwife will advise you on an iron-rich diet or prescribe iron replacement therapy if you develop anaemia during the pregnancy.
During the appointment, your body weight and arterial blood pressure will be measured. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema and will perform a fetal cardiotocography (CTG) to assess your child's well-being and your uterine contractions.
The midwife will advise you on the results of the CTG. She will discuss with you the preparation for childbirth and advise you to familiarize yourself with the maternity ward where you want to give birth. If you wish, the midwife will give you recommendations for finding an individual midwife for childbirth and will help you to prepare a written delivery plan. If necessary, you will be advised about any discomforts you may experience during the second half of the pregnancy.
The midwife will assess your risk of developing deep vein thrombosis again. If you have an increased risk of developing deep vein thrombosis, the midwife will teach you the subcutaneous injection technique, and your doctor will issue you a digital prescription for low-molecular-weight heparin.
After your appointment with the midwife, the gynaecologist and nurse will perform an ultrasound to assess your child's growth and well-being. This ultrasound examination provides an opportunity to find out if your child has not reached its growth potential in the womb and will require more frequent monitoring and, if necessary, an earlier induction of labour. This ultrasound examination is especially important for women who are at risk of child growth restriction.
If you have been diagnosed with child growth restriction and the child’s condition requires an early induction of labour, your gynaecologist will perform an ultrasound-based fetal lung maturity assessment using a special quantusFLM test. If your child's lungs are still immature and still contain too little surfactant (a surface-active agent that helps keep the alveoli open), your child's lungs will be prepared with betamethasone injections which will be administered to you as intramuscular injections. When the baby's lungs have reached maturity, you will be referred to a maternity hospital to induce labour.
If you are at risk of preterm birth and the CTG performed by the midwife detects irregular uterine contractions, your gynaecologist will perform a vaginal examination with the PartoSure test on the cervix to distinguish false labour from real contractions. When contractions start, you will be sent to the maternity hospital.
During the ultrasound in the thirty-second week of pregnancy, the risk of late preeclampsia can also be assessed. If you are at high risk of preeclampsia, your gynaecologist will draw up an individual monitoring plan for you and your child for the timely detection of preeclampsia. If you develop high blood pressure, the diagnosis will be clarified and antihypertensive treatment will be started in a timely manner along with more frequent monitoring of you and your child. You will be taught home blood pressure monitoring and timely recognition of preeclampsia symptoms.
-
Week 36 of pregnancy

During the appointment, the midwife will perform a urine test and take a blood sample to assess the level of haemoglobin in your blood. Your body weight and arterial blood pressure will be measured at the appointment. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema, and she will perform a CTG to assess your child's well-being and uterine contractions.
Beta-hemolytic streptococcus (GBS) may be present in the genital tract of an expectant mother. After delivery, the microbe is associated with uterine inflammation or, in the newborn, as a causative agent of meningitis or sepsis. Women giving birth who are carriers of GBS receive prophylactic antibiotic treatment at the maternity hospital at the start of labour to prevent the complications described above. You can discuss the necessity for a GBS test with your midwife.
The midwife will teach you how to recognize the signs that labour has begun and how to behave at home if your water breaks prematurely. The midwife will also give advice on when to go to the maternity hospital and what to take with you to the hospital.
After your appointment with the midwife, the gynaecologist and nurse will perform an ultrasound to assess your child's growth and well-being. This ultrasound examination provides an opportunity to find out if your child has not reached its growth potential in the womb and if your child is in breech presentation. If the fetus is in a breech position, the mother will be offered an external cephalic version, which is performed in the hospital where the woman wishes to give birth. Rotating the child to cephalic presentation is successful in half of the cases, which then allows the mother to give birth naturally.
With your consent, your gynaecologist will swab between your labia in order to perform a GBS test.
If you suspect that you have a premature rupture of membranes, your gynaecologist will perform a vaginal Actim PROM test to assess the presence of amniotic fluid. In the event that your water has broken, you will be transferred to a maternity hospital.
During the 36th week of pregnancy, all women are offered a risk assessment for late preeclampsia. The gynaecologist will also prepare a preliminary birth management plan for you. If you require a planned caesarean section, he will give you a referral to the maternity hospital.
-
Week 38 of pregnancy
During the appointment, the midwife will perform a urine test and also take a blood sample to assess the level of haemoglobin in your blood. Your body weight and arterial blood pressure will be measured at the appointment. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema, and she will perform a CTG to assess your child's well-being and your uterine contractions.
The midwife will advise you on the postpartum adjustment, breastfeeding and newborn care and will discuss with you whether it would be better to continue to monitor the newborn after delivery with a family doctor or paediatrician.
-
Week 40 of pregnancy
During the appointment, the midwife will perform a urine test and take a blood sample to assess the level of haemoglobin in your blood. During the appointment, your body weight and arterial blood pressure will be measured. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema, and she will perform a CTG to assess your child's well-being and uterine contractions. The midwife will advise you on the postpartum period and on when to come to the gynaecologist for a postpartum examination. The midwife will offer reassurance that if you have problems with breastfeeding after the delivery, you are always welcome to come and see her.
-
Week 41 of pregnancy
During the appointment, the midwife will perform a urine test and take a blood sample to assess the level of haemoglobin in your blood. During the appointment, your body weight and arterial blood pressure will be measured. During the visit, the midwife will express interest in the nature of your child's movements and the presence of oedema, and she will perform a CTG to assess your child's well-being and uterine contractions.
After the appointment with the midwife, the gynaecologist will assess via vaginal ultrasound examination and palpation the length and maturity of the cervix and the possibility for spontaneous delivery.
In the case of an immature cervix, the gynaecologist will start with your consent preparing your cervix with a vaginal progesterone gel.
If there are deviations from the normal course of pregnancy: tests during pregnancy are not in order, it is a high-risk pregnancy or if you have an internal medical condition, the pregnancy monitoring and screening intervals will depend on the specific case. Dichorionic (with two placentas) twins are monitored by a gynaecologist along with a midwife at 4-week intervals, and monochorionic twins at 2-week intervals.
However, fetuses with growth restriction need to be monitored at either two- or one-week intervals, depending on the child's well-being.
In cooperation with the best specialists in their field, you will be referred to a 3rd level hospital for further testing and treatment, if necessary.

For women registered at the Fetal Ultrasound Center, all ultrasound examinations are 10% cheaper after registration for pregnancy.
When you have given birth, please write to our midwife ammaemand@ultraheli.ee about how the delivery went, how much your baby weighed at delivery and what Apgar score it received.
We recommend that you schedule an appointment with Dr Marek Šois for a postpartum check-up eight weeks after delivery. If you had to undergo a caesarean section or developed gestational diabetes, severe anaemia, high blood pressure or preeclampsia during your pregnancy, it is recommended that you schedule a postpartum check-up earlier.
Read more:
Why you might consider registering with a Fetal Ultrasound Center

