Fetal Ultrasound Centre offers the RhSafe test for a non-invasive assessment of fetal rhesus status
Rhesus factor (Rh) is one of the most critical blood group systems. On the surface of human red cells are the protein antigens that make up the rhesus factor. Of RH antigens, the most clinically important is antigen D. People with the RhD antigen on the surface of red cells are RhD positive, and those without it are RhD negative. There are about 15% of RhD-negative people in Europe.
Why is it essential for me to know my RhD affiliation during pregnancy?
The Rhesus factor is crucial during pregnancy. If the mother is RhD positive, there is no RhD conflict whether her child is RhD positive or RhD negative. If the mother is RhD negative and the child is RhD positive, a Rhesus conflict may occur, in which the mother's immune system produces antibodies to the child's RhD-positive red blood cells.
What does it depend on if my child is RhD positive or RhD negative?
Whether a child is RhD positive or negative depends on the father. If the father has a dominant rhesus allele (40% of cases), then his offspring are all RhD positive, whereas if the father has a recessive allele (60% of cases), half of his offspring are RhD positive and half are RhD negative.
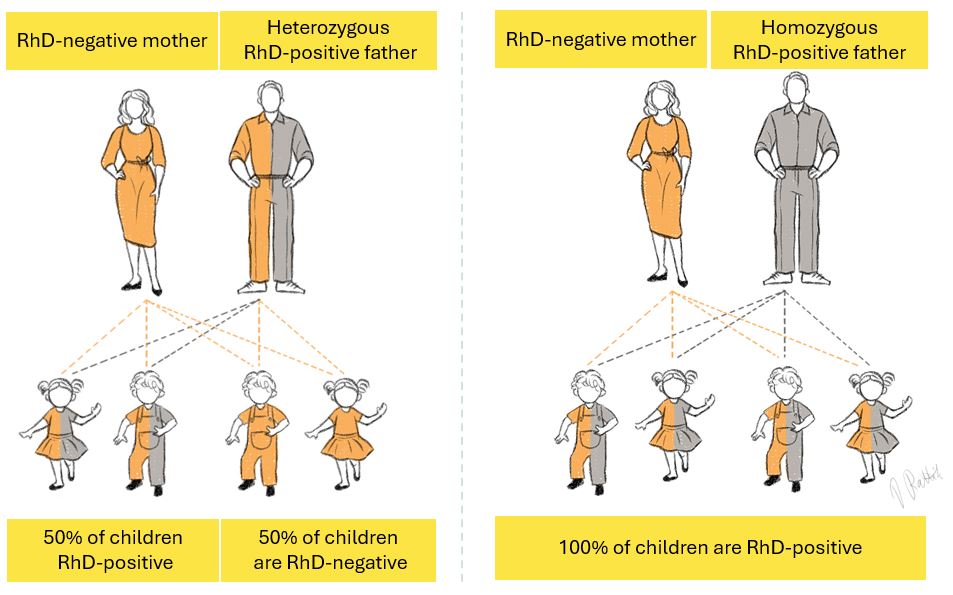
Figure 1: Inheritance of the Rhesus factor depending on whether the child's father has a dominant or recessive Rhesus allele.
Why and how will there be a rhesus conflict?
A rhesus conflict occurs when the mother's and child's blood are exposed to each other for specific reasons, such as during childbirth, miscarriage, fetal water breakage, external fetal twists, trauma, or bleeding. Only a minimal amount of RhD-positive blood is needed to induce immunisation; as little as 0.1 ml is sufficient. During pregnancy, there is also occasional mixing of foetal and maternal blood, mainly after the 28th week of pregnancy or during the third trimester.
If rhesus incompatibility occurs, a small amount of foetal blood enters the mother's bloodstream, prompting her immune system to produce anti-D antibodies against foetal red blood cells, leading to haemolytic disease in the foetus.
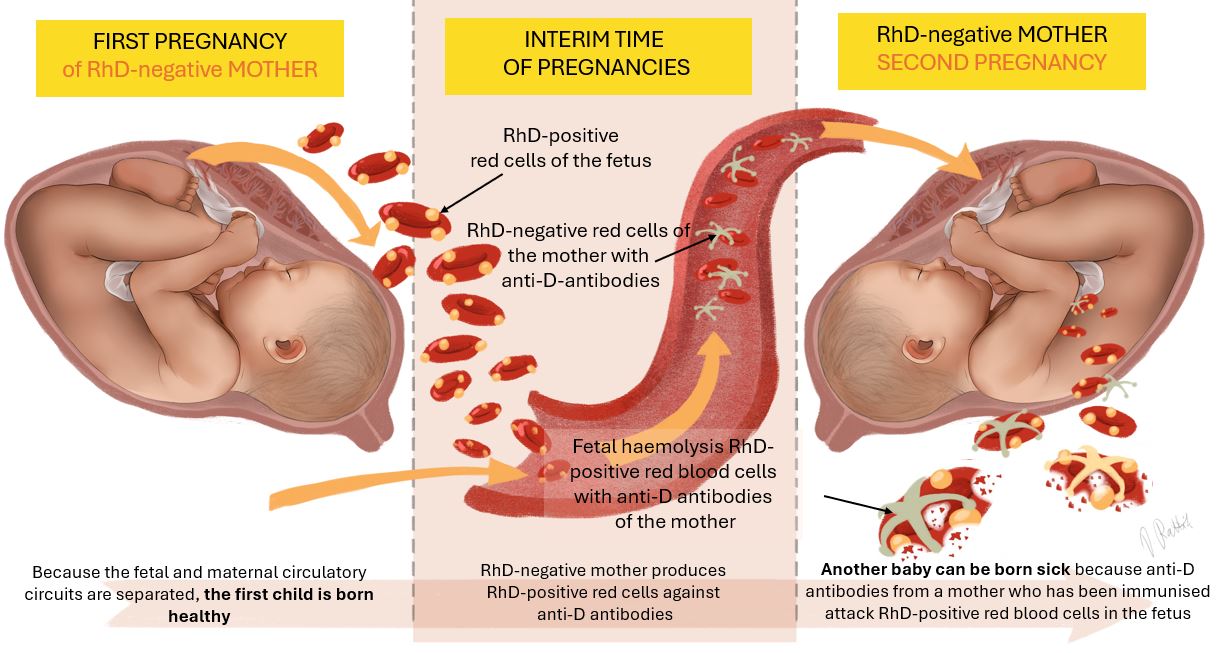
Figure 2: Mechanism of pathogenesis of hemolytic disease in an RhD-positive fetus of an RhD-negative mother.
What is foetal haemolytic disease?
By entering the fetal bloodstream, antibodies bind to antigens on the foetal red cells, causing haemolysis and a low number of red cells (anaemia) in the fetus. Red blood cells contain haemoglobin, which binds oxygen needed for life and transports it to all body organs. However, as red blood cells break down, the oxygen supply to fetal organs and their function declines. Due to the extensive breakdown of red cells, heart failure develops, worsening the oxygen deficiency in the child's brain and increasing the production of red cells in the liver. This can, in turn, lead to life-threatening swelling of fetal tissue.
Why do you need to know the child's rhesus?
If the mother lacks anti-D antibodies, anti-RhD prophylaxis can be administered to the RhD-positive baby at 28 weeks of pregnancy. This is achieved using anti-D immunoglobulin Rhesonativ, whose antibodies prevent the mother's immune system from developing its own anti-D antibodies, thereby preventing haemolytic disease in the foetus. Women who received Rhesonativ before delivery will receive a second dose of anti-D immunoglobulin within three days after giving birth. In 40% of cases, the child of an RhD-negative woman is also RhD-negative, and the mother does not require anti-D prophylaxis.
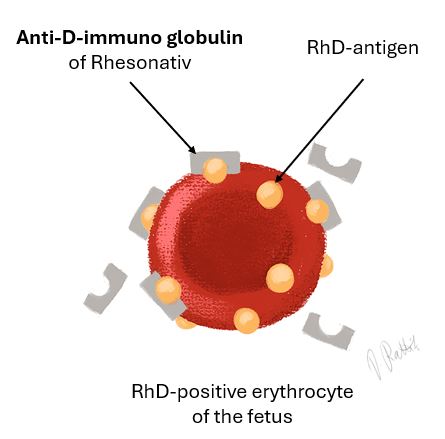
Figure 3: Rhesonativ's effect on blocking antibodies on the surface of red blood cells
If the mother already has anti-D antibodies, it is essential to determine the titre level in the case of an RhD-positive foetus. If this value is very high, ultrasound Doppler assessment of the central artery of the fetal brain should be carried out to evaluate the presence and severity of fetal anaemia. In cases of severe fetal anaemia, a life-saving intrauterine transfusion can be performed before birth. In exceptional circumstances, early delivery may be necessary. However, if an RhD-negative woman is carrying an RhD-negative child, she can be reassured that her baby cannot develop haemolytic disease.
How can you find out whether a fetus belongs to rhesus?
It is possible to determine foetal RhD status during pregnancy using the RhSafe test. The RhSafe test is a non-invasive prenatal screening procedure that is safe for both the mother and the baby. The results are available 14 working days after the blood sample has been taken.
How does the RhSafe test work?
The RhSafe test is performed using a mother's blood sample containing both maternal and foetal DNA. The test detects fetal DNA in the mother's blood and confirms the presence of exons 5 and 7 of the fetal RhD gene through PCR analysis. If the fetus has an RhD gene, it is RhD positive; if the gene is absent, then the fetus is RhD negative.
How reliable is the RhSafe test?
This screening can detect 99.9% of all RhD-positive fetuses and 99.1% of all RhD-negative fetuses.
Who can be tested and when?
The RhSafe test will only be performed for mothers who are RhD negative and whose child's father is RhD positive. The RhSafe test can be offered to mothers whose pregnancies have lasted at least 10 full weeks (10 weeks + 0 days). The fetal rhesus factor can only be determined from the fetal blood for single pregnancies. If you would like to know the duration of your pregnancy, please visit our pregnancy calculator.