The Fetal Ultrasound Centre offers early combined fetal developmental screening
Video.10 weeks pre-NIPT ultrasound. Dr Marek Šois 2023
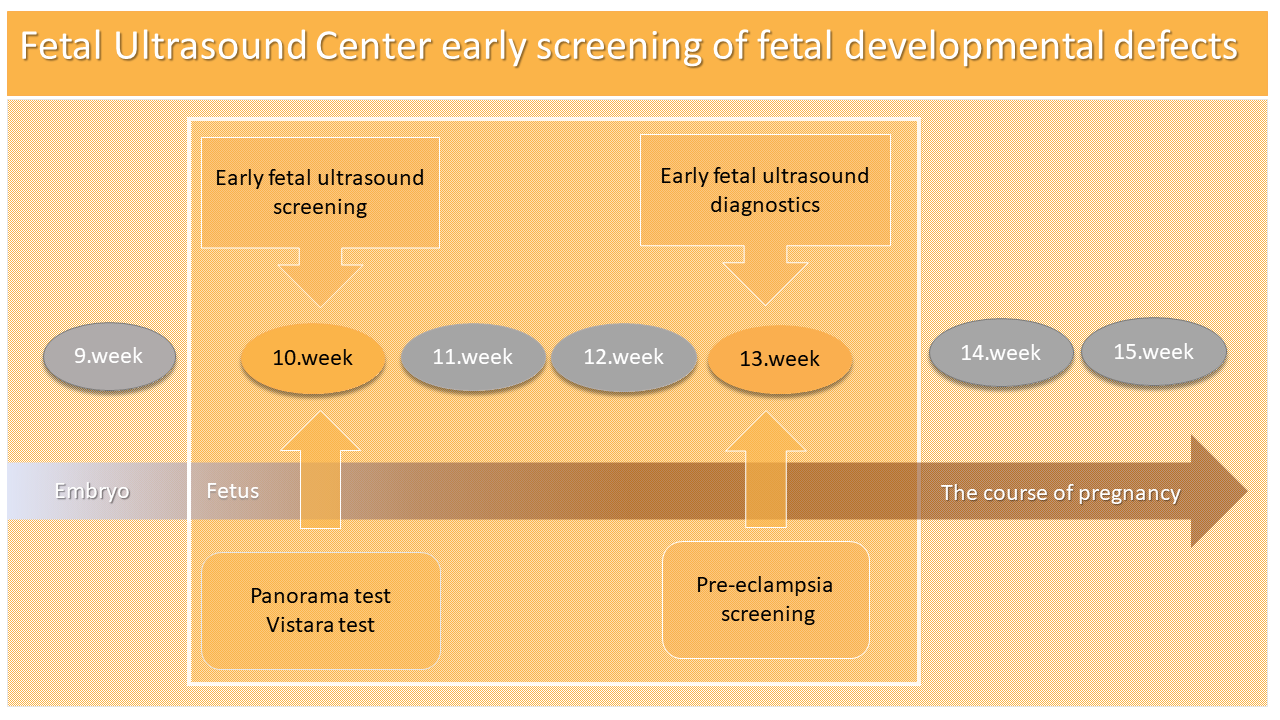
“A very early ultrasound examination of fetal developmental defects with an extracellular DNA test (NIPT) at 10 weeks of pregnancy, combined with an OSCAR test at 13 weeks of pregnancy, is currently the most accurate combined prenatal screening method for an early detection of chromosomal diseases and developmental defects,” says gynecologist Dr. Marek Šois.
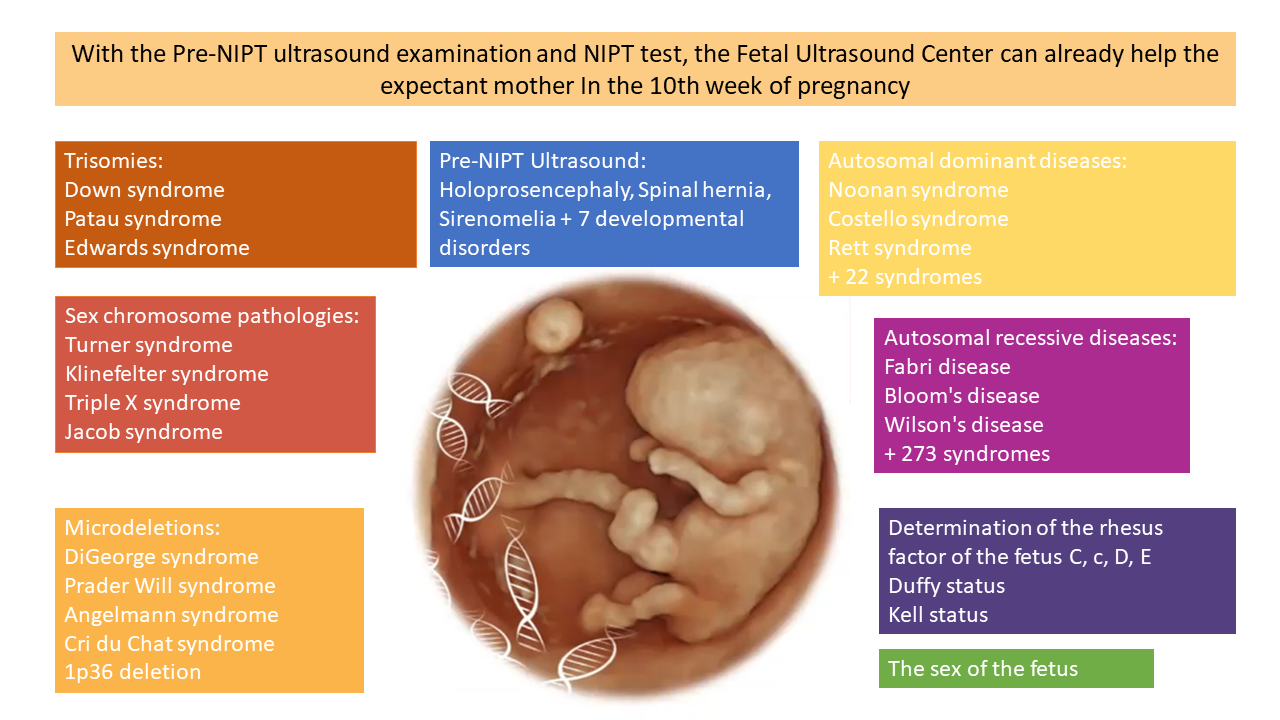
The Panorama test can detect fetuses with Down, Edwards, Patau and Turner syndromes, X-chromosome gene mutations and microdeletions. The Visara test can provide information on the pathology of 30 single genes in the fetus, which can cause 25 different genetic diseases that a prenatal ultrasound cannot detect. The frequency of fetal chromosomal diseases depends primarily on the age of the mother, while the frequency of monogenic diseases depends on the age of the father. Dr. Šois points out the differences between the Panorama test and the Vistara test: "Therefore, if the mother is over 35 years old, it is wise to take the Panorama test, but if the father is over 40 years old, it is wise to take the Vistara test in addition to the Panorama test."
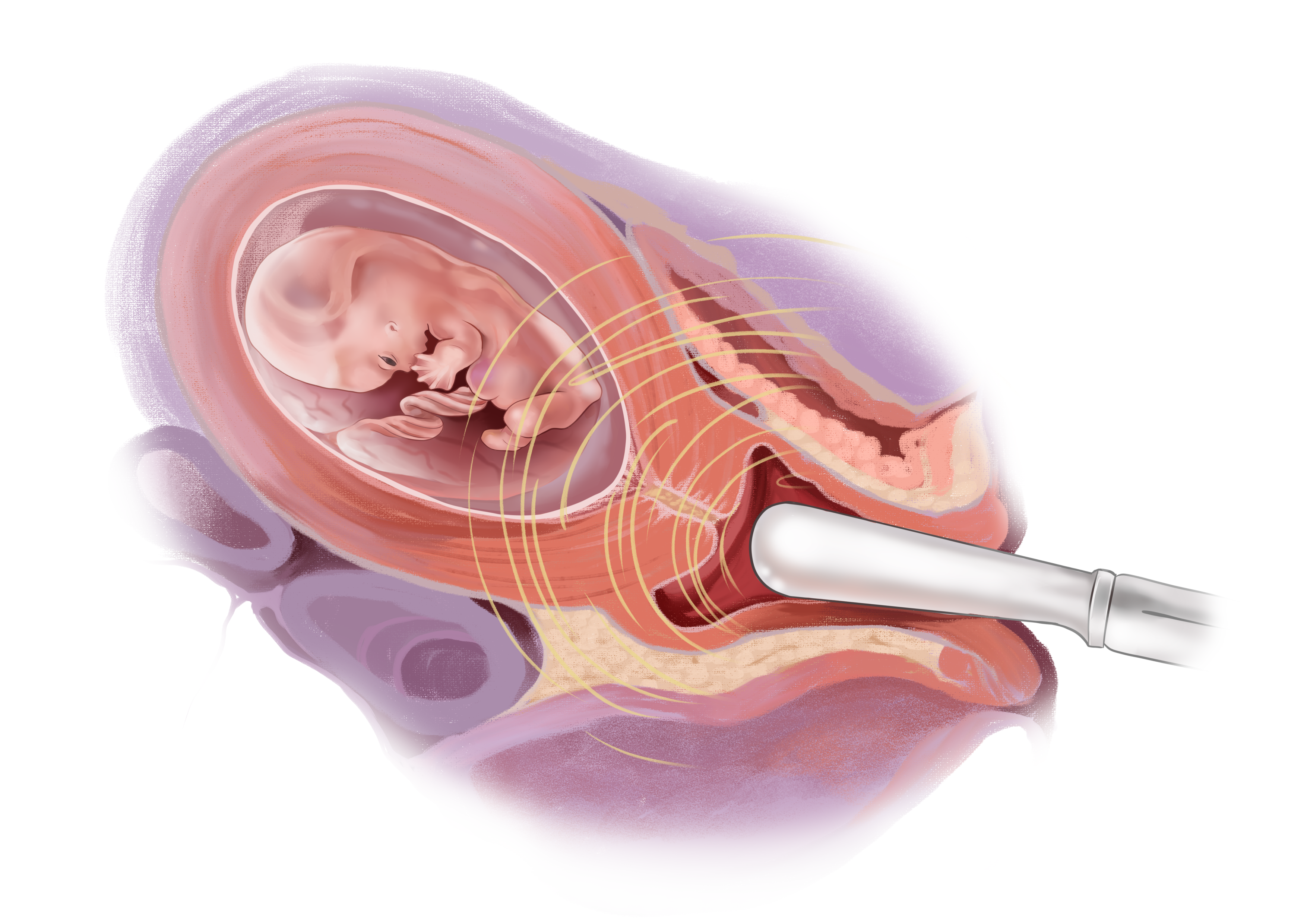
An ultrasound examination of fetal developmental defects prior to the NIPT test is performed from the 10th week of pregnancy, when the fetus is already 32 mm in length. In a pregnancy of this size, the embryonic period of the fetus has ended, and they have already developed the main organ structures that can be assessed during the mother's vaginal ultrasound examination.
Fetal vaginal ultrasound at week 10 of pregnancy
The purpose of an ultrasound scan is to first determine the size of the pregnancy, to assess the presence and type of a possible double pregnancy, and then to exclude situations in which the NIPT test should not be performed.
The NIPT test should not be performed in the following cases:
- The duration of the pregnancy is less than nine weeks;
- Miscarriage;
- The death of one twin;
- Major developmental disorders of the child;
- A large nuchal fold of the fetus (NT > 3.5 mm).
In 1 out of 10 cases, a pre-NIPT ultrasound examination changes the way the screening test is performed. The older the mother, the more important the pre-NIPT ultrasound examination.
- If the pregnancy is less than nine weeks, the NIPT test should be postponed;
- If there's been a miscarriage, if one of the twins has died, if there are triplets, or if the child has major developmental disorders, the NIPT test cannot be performed;
- The Vistara test cannot be performed in case of a double pregnancy.
- The PanoramaXP test cannot be performed for dichorionic twins, but only the Panorama 22q11 test can be performed for monochorionic twins;
- If the fetal nuchal fold exceeds 2.2 mm in size, immediate NIPT testing is not warranted. In this case, it is reasonable to repeat the ultrasound examination at the 12th week of pregnancy. If the thickness of the nuchal fold has not increased during the repeated ultrasound examination, then the NIPT test can be performed;
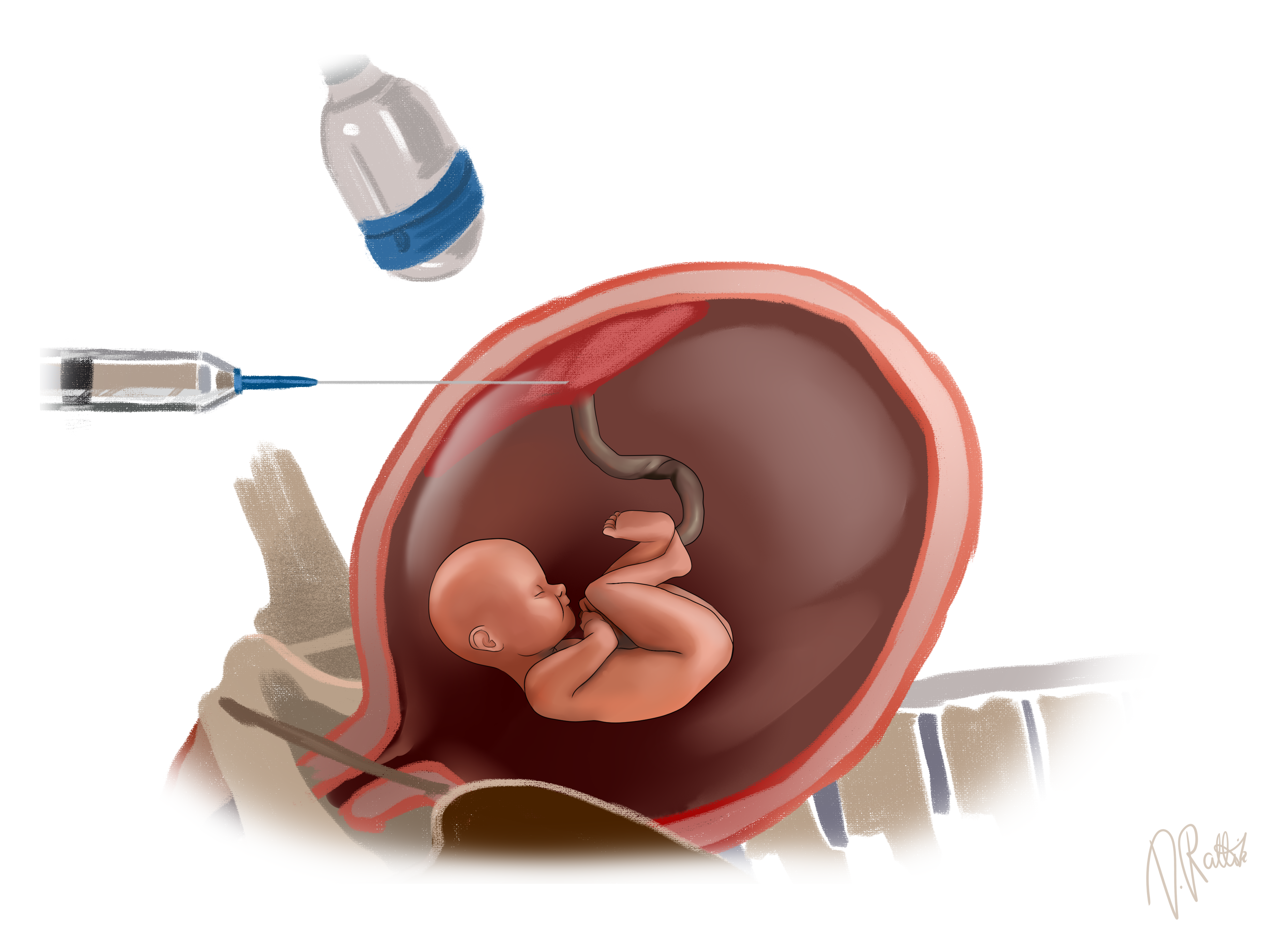
- If the fetal nuchal fold exceeds 3.5 mm in size, immediate NIPT testing is not warranted. In this case, Dr. Šois will perform a chorionic biopsy at the Fetal Ultrasound Centre with the consent of the family. This is done, because a fetus with an enlarged nuchal fold has an increased risk for Down syndrome, as well as another 200 different chromosomal and genetic diseases that cannot be detected by the NIPT test.
The chorionic biopsy will be performed at the Fetal Ultrasound Centre during weeks 11-14 of pregnancy.
Since the NIPT test cannot detect structural developmental defects in a child, the objective of the pre-NIPT ultrasound examination is to exclude 10 severe developmental defects in the child, which are the following:
- Absence of skull bones (incidence 1: 1000);
- Absence of cerebral hemispheres (incidence 1: 1300);
- Spinal hernia (incidence 1: 2000);
- Absence of arms, hands, legs or feet (frequency 1: 2000);
- Cranial hernia (incidence 1: 5000);
- Large umbilical hernia, due to which the liver is located partly outside the body through the navel (incidence 1: 3500);
- Amniotic cord syndrome (incidence 1: 7000);
- Severe anterior abdominal wall defect with visceral organ attachment to the placenta (incidence 1: 7500);
- Sirenomelia or mermaid syndrome (fused legs) (frequency 1: 60000);
- Conjoined twins (1% of monochorionic twins).
In the case of the above-mentioned severe developmental disorders of the child, the woman has the right to terminate the pregnancy without performing prenatal invasive examinations. In this case, a chromosomal examination of the aborted fetus with the consent of the family after the termination of the pregnancy is a reasonable intervention.
In order to ensure a safe course of pregnancy for the pregnant woman and the confidence that she will bear a healthy child, Dr. Marek Šois recommends combining an ultrasound examination for very early fetal developmental defects with NIPT tests, along with the OSCAR test carried out between the 12th and 14th week of pregnancy.
If a woman has previously taken the NIPT test, then by the time she comes to the OSCAR test, she will know whether the child will be a boy or a girl, and that the fetus does not have the most common chromosomal or genetic diseases. Therefore, as part of the OSCAR test, the gynecologist can focus on the detailed assessment of fetal organ structures and conduct an early ultrasound examination of fetal developmental defects, which can be used to exclude more than 100 different developmental defects, including life-threatening severe heart defects and neural tube pathologies (cerebral hernia, spinal hernia, anterior abdominal wall pathology).
In special cases where a single fetus has died during a double pregnancy or a triple pregnancy and the NIPT test cannot be performed, or the NIPT test has failed due to a low amount of cellular DNA in the mother's blood, the OSCAR test is the only possible method to assess the risk of Down syndrome.
In addition, the OSCAR test can also assess a pregnant mother's risk for the most serious pregnancy complication - preeclampsia, which causes the birth of a preterm infant who is not yet able to breathe, maintain a temperature, or fight infections outside the uterus. A mother at a high risk for preeclampsia can start taking low-dose aspirin in a timely manner, which in 90% of cases prevents the development of preeclampsia and a very premature birth (before 32 weeks of pregnancy).
In any case, whether through a chromosome analysis or an ultrasound, it is important to get a complete idea of the health of the fetus as early as possible during the pregnancy. "If the worst-case scenario materializes and the expected child turns out to be ill, the parents will have the opportunity to decide whether to still give birth or terminate the pregnancy. If the parents decide to terminate the pregnancy, it is important to do so as early as possible - it is less traumatic both physically and mentally," explained Dr. Šois.